What Do New BP Guidelines Mean For You?
 The American College of Cardiology and the American Heart Association partnered to review and update clinical guidelines for the prevention, detection, evaluation and management of high blood pressure (HBP). They were joined by a number of organizations representing physicians and other health professionals in this endeavor including the American Academy of Physician Assistants, American Pharmacists Association, and American Society of Preventive Cardiology.
The American College of Cardiology and the American Heart Association partnered to review and update clinical guidelines for the prevention, detection, evaluation and management of high blood pressure (HBP). They were joined by a number of organizations representing physicians and other health professionals in this endeavor including the American Academy of Physician Assistants, American Pharmacists Association, and American Society of Preventive Cardiology.
Under the old guidelines, 32% of American adults were considered to have hypertension, or HBP, meaning the patient’s blood pressure (BP) readings continued to be at 140 mm Hg systolic or 90 mm Hg diastolic, or higher. AMA Vice-President of Chronic Disease Prevention and Management, Michael Rakotz, MD, says the new guidelines are the “most significant” since 2003. There have been updates to portions of the guidelines, but compared to the recent revisions, Rakotz states, “none that were as comprehensive as this new guideline.” The authors wrote the “guidelines are intended to define practices meeting the needs of patients in most, but not all, circumstances and should not replace clinical judgment.”
The new 2017 hypertension guidelines lower the threshold to 130/80 mm Hg. This change means that approximately 46% of American adults will be considered to have HBP. These patients are not at higher risk than they were a few months ago, but their risk factors are being identified earlier in an effort to promote positive changes before catastrophic events such as strokes, heart attacks and other cardiac problems occur.
AMA President, David O. Barbe, MD, MHA, points out, “High blood pressure can often be managed effectively when patients work with their physician to create a treatment plan that focuses on healthy lifestyle changes such as exercising, eating a healthy diet, reducing salt intake, drinking alcohol in moderation, losing weight if overweight, and using anti-hypertensive medication when needed.”
Here are a few things you need to know about the new guidelines and how it may affect you.
First, there are now 4 categories of BP readings: normal, elevated, HBP (hypertension) Stage 1, and HBP (hypertension) Stage 2 as illustrated in the AMA graphic below.
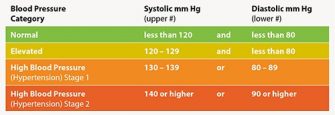
In order to determine an individual’s category, readings from two separate occasions should be averaged. In the event a person’s readings for systolic and diastolic are not in the same category, the higher risk category would be used. It is also beneficial to have confirmation of the elevated BP outside of the normal office visit.
The lower threshold means a large number of people who were previously considered “normal” will now be classified as “Elevated” or “Stage 1”. This does NOT mean they should all seek blood pressure medication immediately.
For many patients, lifestyle changes will be sufficient to bring them back down to the “Normal” classification. Weight loss, increasing physical activity, lowering sodium intake, proper stress management and other small changes can make a significant difference in blood pressure. For example, a 10-pound weight loss can lower BP by as much as 5 mmHg.
The AMA recommends “All patients with high BP should be treated with non-pharmacological interventions, which include weight loss for those who are overweight or obese, a heart-healthy diet such as the dietary approaches to stop hypertension (DASH) eating plan, sodium reduction, potassium supplementation (under the guidance of a physician), increased physical activity with a structured exercise program, and drinking alcohol in moderation.”
The addition of BP-lowering medication is based on the stage of hypertension, a patient’s individual medical history or their estimated 10-year Cardiovascular Disease (CVD) risk that is 10% or higher (using the ACC/AHA Risk Estimator). Including factors such as age to identify who might benefit from medication along with the lifestyle changes is a change from previous guidelines.
In another break from the past, treatment goals are now more tailored to the patient’s individual health. For instance, a patient who already has CVD or a 10-year risk that is greater than 10% may have had a goal of BP that was 130/80 mm Hg or lower. At the same time, a person with no risk factors may have still been advised to keep their BP to 120/80 mm Hg or lower. Under the new guidelines, for some with no risk factors, a target of 130/80 mm Hg may still be considered reasonable.
The new guidelines also place emphasis on patients self-monitoring BP. It is very common for office BP measurements to be higher than those taken at home or in an ambulatory setting. Self-monitoring, when combined with telehealth counseling or clinical interventions, helps to confirm the diagnosis as well as allows for more scrutiny when BP-lowering medication dosages are being changed. Furthermore, self-monitoring may help distinguish between sustained, white coat and masked hypertension. The guidelines do note that any self-monitoring should be done with a reputable device that has utilizes proper protocol.
As with any health issue, basic guidelines do not account for all patients. Individuals have a wide range of history, habits and other factors that will affect their health and how they respond to a treatment. The emphasis the new guidelines places on prevention and self-care goes hand in hand with overall wellness.
In addition to checking your BP when you are in the office, your doctor of chiropractic is an excellent source of information on exercise, nutrition and other lifestyle changes you can make that may help lower your BP and other risk factors. Find a doctor near you as well as articles on wellness at tnchiro.com.
SOURCE: “New BP guideline: 5 things physicians should know” on the AMA Wire
https://wire.ama-assn.org/delivering-care/new-bp-guideline-5-things-physicians-should-know
Nov 13, 2017 by Sara Berg Senior Staff Writer